Incision and Drainage
Preparation, Procedure Steps, After Care and Followup
Preparation
- Goggles
- Sterile gloves
- Chlorhexidine (or other approved skin cleanser)
- Local anesthetic, syringe, needle (see chapter titled “Local Anesthesia” for full procedure)
- Laceration tray
- 30mL syringe and 16-guage IV cathlon (for irrigation)
- Kelly forceps
- Sterile saline
- No. 11 scalpel
- Packing material
- Absorbent dressing (such as Mepore)
- Culture swab and medium
- Microbiology requisition
Procedure Steps
Step 1: Health history and physical examination
Assess the duration the lesion has been present, location, allergies, bleeding disorders, and risk factors for poor wound healing. The procedure should only be performed with an abscess that is within the skin and subcutaneous tissue with palpable boundaries.
Step 2: Cleanse the area with chlorhexidine
Wound cleansing reduces risk of sepsis to the wound site. Cleanse a wide area around the wound to prevent contamination of suture material and surgical instruments during the procedure.
Step 3: Anesthetize the area
Use a field block technique to anesthetize the area. Tissue around an abscess is acidotic making local anesthetic less effective; therefore, ensure the field block around the abscess is about 1 cm from the erythema. Using anesthetic with epinephrine will constrict blood vessels and decrease bleeding during the procedure. Avoid use of epinephrine in the digits, ears, and nose due to the risk of ischemia.
Another approach is the use of topical anesthetic, such as ethyl chloride sprayed on the site where the incision will be made.
Reassure the patient that the pain will decrease once the pressure is relieved.
Use a needle prick to check for sensation.
Step 4: Drape the site
Have extra 4×4 gauze to absorb drainage.
Step 5: Open the abscess
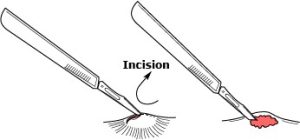 Using a number 11 scalpel blade open the abscess directly over the center of the abscess along existing skin-tension lines and allow the purulent matter to drain under its own pressure.
Using a number 11 scalpel blade open the abscess directly over the center of the abscess along existing skin-tension lines and allow the purulent matter to drain under its own pressure.
Use a quick decisive motion to minimize patient discomfort.
The incision must be sufficiently wide to allow appropriate drainage and to prevent premature closure of the incision.
Apply pressure to the area to assist with expression of pus and the abscess contents.
Step 6: Perform blunt dissection
Perform blunt dissection of the abscess cavity and break up any pockets of purulent matter using Kelly forceps or sterile cotton-tipped applicator.
Step 7: Irrigate
Gently irrigate the abscess with saline until all purulent matter is removed.
Step 8: Insert packing material
Avoid overpacking the wound; this may cause ischemia of the surrounding tissues and impede the desired drainage of purulent material
Packing material should keep the walls of the abscess separated and allow further drainage of infected debris while preventing premature closure of wound which can lead to re-accumulation of bacteria and recurrent abscesses.
Step 9: Apply dressing
Apply a dressing that will effectively manage drainage.
Video
Video
Aftercare
- Advise the patient to keep the site clean and dry – cover with dry gauze until fully healed
- If no packing in place, soak the wound in warm soapy water several times per day and then cover with dry gauze
- Instruct patient to monitor for signs and symptoms of infection:
- recollection of pus in abscess
- fever and chills
- increased pain and redness
- red streaks near the abscess
- increased swelling
Patient Education
Follow-up
Schedule patient to return in 24-48 hours post procedure. If packing was used the packing needs to be changed daily until purulent drainage has stopped and granulation tissue is present. Once packing is no longer needed, instruct the patient to do warm wet soaks several times per day until healing is completed.
Key Takeaways
- Cultures are not recommended for non-purulent lesions. Culture when pus or purulent drainage is present and there is suspicion for MRSA; or when there is systemic illness.
- Routine use of oral antibiotics after uncomplicated I&D is not recommended.
- Antibiotics should only be used for patients with complicated abscesses (those having systemic symptoms), immunocompromised patients, and for abscesses with significant surrounding cellulitis or in areas that are difficult to drain, such as the hand.

