Speculum Exam and Papanicolaou (PAP) Smear
Preparation, Procedure Steps, After Care and Followup
Preparation
- Appropriate style/size of speculum (see discussion below)
- Light source
- Warm water or water-soluble lubricant
- Non-sterile gloves
- Cytobrush and spatula
- Liquid-based cytology container
- PAP requisition
- History checklist, reason for the Pap smear, any abnormalities noted (e.g., herpes, vaginal infection), the sampling tools used and LMP, pregnancy, date of menopause, and current contraceptive use.
- You may wish to have culture swabs for BV/Candida available in case of client complaints of discharge or odour, or in the event that you note unusual findings on exam.
Speculums
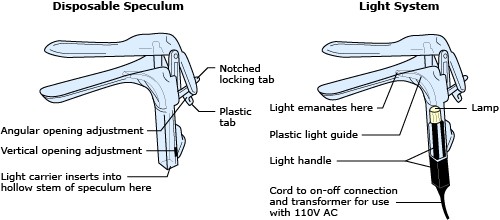
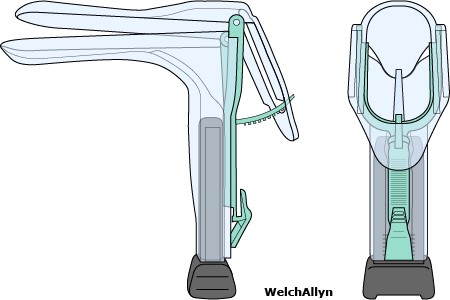
It is essential that you become thoroughly familiar with how the speculum operates before you begin the examination. In your review, be sure to include the disposable plastic speculum (see figure below), since the mechanism action of this type of speculum is somewhat different. Plastic specula typically make a loud “click” when locked or released; therefore, please forewarn your patient about this click to avoid surprise and unnecessary anxiety.
The speculum consists essentially of two blades and a handle. Two views are shown below, and a discussion of individual parts follows.
Examine the blades first.
- The upper and the lower blade can each be divided into three parts: a base, a body and a tip.
- The two blade bases together may be called the base of the speculum.
- The speculum base is flared and forms a viewing aperture.
Next, look at the three pieces added to, or extending from, the bases of the blades.
- The first–a lever extending from the base of the upper blade–may be called the speculum lever (or notched locking tab or thumbplate). The angular opening adjustment holds the speculum open when the notched locking tab is pressed down.
- The others–a Y-shaped piece attached to the base of the upper blade, and an L-shaped piece extending from the base of the lower one–together make up the speculum handle.
- The vertical opening adjustment is used to extend the viewing aperture. It can be slid down to open the aperture wider. This is a useful technique when vaginal walls are flaccid and fall into themselves.
Some sites utilize a metal speculum. These have a rod inserted through the lever and attached to the handle. The rod is threaded and carries a nut, and the two pieces may be called the lever rod and lever nut (or adjustment screw), respectively. Finally, note the bolt similarly inserted through the two components of the handle and also carrying a nut–these two pieces may be called the handle bolt and handle nut, respectively. These are demonstrated in the depiction of the Graves and Pederson specula below.
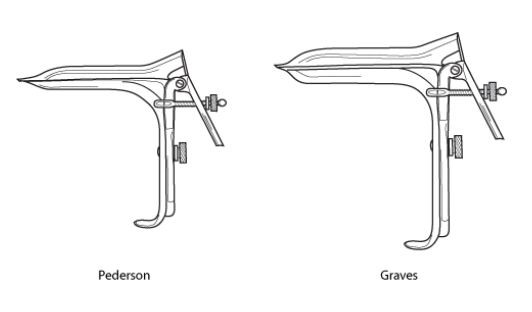
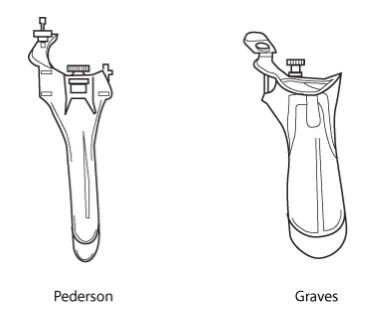
After the health history, you will have an idea of the appropriate type and size of speculum needed. There are two basic types: the Graves specula, and the Pederson speculum (see figures above).
The Graves speculum is most commonly used for the adult female client. It varies in length from 9-13 cm and is 4 cm wide. Most of the disposable specula that are available are Graves specula and come in small, medium and large sizes. The Pederson speculum is both narrower and flatter than the Graves speculum, and it is used with virgins, nulliparous patients, circumcised patients, or patients whose vaginal orifices have contracted postmenopausal. They will need to be special ordered.
The Pap is best performed when the patient has had:
- no heavy menstrual bleeding (i.e., mid-cycle; day 10-20 sampling is ideal)
- nothing in the vagina for at least 24 hours; this includes: no intercourse, douching, vaginal medications, or contraception (except for the NuvaRing; Hatcher et al., 2004)
Procedure Steps
Step 1: Insertion of speculum
(i) Have the patient void prior to the examination
This will minimize discomfort.
(ii) At the time of insertion, both the blade tips and bases should be aligned and secured in a closed position
In a metal speculum, the handle nut should be loosened, the blades aligned, then the handle nut tightened.
(iii) Warm and lubricate the speculum with lukewarm water.
The use of lubricants during sampling is discouraged as it may interfere with sample processing and yield an unsatisfactory result. If used, apply a tiny amount of lubricant on the speculum’s exterior. Avoid covering the tip with lubricant to avoid getting lubricant on the cervix.
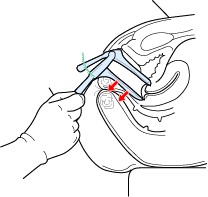
(iv) Grasp the speculum and spread the labia majora

With gloved hands grasp the speculum in the dominant hand and use the other hand to spread the labia majora. Hook the index finger of the dominant hand over the base of the upper blade, to make your grasp firmer. Open the introitus (i.e., vaginal orifice) by spreading the labia majora from above, or from below, while applying downward pressure.
(v) Insert the speculum

To provide for a smooth insertion, unimpeded by the vaginal walls, orient the speculum blades along the axis of the vaginal canal.
The vaginal axis runs from above to below the horizontal when a woman is in the lithotomy position.
Note that the blade tips should be placed against the lower (i.e., posterior) wall of the vagina, rather than the anterior wall, to avoid contact with the urethra. Ask the patient to take a deep breath to relax her vaginal orifice.
Hold the speculum with the handles straight down. Insert the speculum with gentle pressure posteriorly.
You may have to continue to spread the labia majora for smooth insertion. As it enters the vagina, maintain gentle pressure backwards along the length of the posterior blade.
(vi) Rotate the speculum

Insert the speculum up to the base then rotate it parallel to the posterior wall of the vagina. This positions the speculum for the first attempt to view the cervix using only the blade tips.
In most women, gentle pressure of the lower base against the perineum is sufficient to place the blade tips in the posterior fornix.
The hand which was separating the labia can now be removed from the labia since it is no longer needed.
(viii) Apply pressure on the speculum
In pressing the lower blade against the posterior vaginal wall, exert pressure uniformly along the entire body of the blade.
If exerting greater pressure on the tip of the blade, the base of the blade acts as a fulcrum at the vaginal orifice–which may cause the base of the upper blade to hit the urethra. Some upward pressure on the anterior vaginal wall is unavoidable.
Step 2: Performing the PAP
(i) Gently wipe away excessive discharge or mucous, if necessary, with a large Q-tip or ring forceps holding a folded gauze pad. Do not touch the cervical os.
(ii) Obtain an ectocervical sample
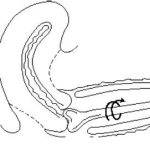
Place the bifid end of the plastic spatula into the os of the cervix.
Use firm pressure and rotate 360 degrees around the cervix, while maintaining tight contact with the ectocervical (outside visible) surface. Include the entire transformation zone. To identify the T-Zone with your naked eye, look for the color change between the red columnar epithelium and the smooth pink mature squamous epithelium. If color changes are identified outside of the area first sampled (360 around the cervix), sample these areas too.
Withdraw the plastic spatula carefully to avoid contamination with the vaginal walls.
(iii) Transfer the sample to the liquid-based cytology solution
Rinse the spatula as quickly as possible into the liquid-based solution vial by swirling the spatula vigorously in the vial 10 times.
Discard the spatula.
(iv) Obtain an endocervical sample
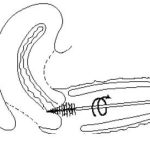
Gently insert the cytobrush deep into the cervical os until only the bottom-most fibers are visible.
Rotate slowly counterclockwise 1/2 a turn and then the other way half a turn and gently remove.
Remove the cytobrush carefully to avoid contamination by vaginal walls.
Over-rotating may damage some cervical cells and often induces more capillary bleeding, which in turn may increase post PAP spotting and temporarily increase the risk of sexually transmitted infections
(v) Transfer the sample to the same liquid-based solution
Rinse the endocervical brush as soon as possible in the liquid-based solution. Rotate the device in the solution 10 times while pushing the brush against the vial wall. Swirl the brush vigorously to further release material.
Discard the brush.
Step 3: Removal of Speculum
(i) Release the speculum lever

Once the cervix has been inspected and appropriate procedures are carried out, the speculum can be withdrawn. Release the speculum lever by pushing upwards on the notched locking tab, causing a clicking sound. It is recommended to warn the patient in advance that she should expect to hear this sound.
(ii) Withdraw speculum and inspect vaginal mucosa

During withdrawal, view the vaginal mucosa by keeping the blade tips partially open with your thumb. Rotating the speculum to either side during withdrawal will allow viewing of the posterior and anterior wall of the vagina. Only a partial opening of the blade tips are warranted for viewing, as a complete opening would unnecessarily distend the vaginal walls.
(iii) Remove speculum

As the blade tips are withdrawn through the vaginal orifice, they should be completely closed to avoid client discomfort. Irritation of the urethra is also a danger during withdrawal of the speculum; therefore, maintain pressure of the lower blade against the posterior wall. The posterior wall is quite resilient and can accommodate considerable pressure without discomfort to the patient. Always check to be certain space exists between the upper blade and the urethra.
Aftercare
- Inform the patient that she may have blood spotting following the procedure and offer a panty liner.
- Record the patient’s name and ID number on the specimen vial and place in specimen bag with completed requisition.
- Transport sample to laboratory.
Patient Education
Follow-up
Inform the patient that she will be contacted and that follow-up will be arranged if her PAP smear is abnormal.
Ensure that the patient understands her future appointment times and dates, and that she understands the importance of follow-up of abnormal PAP results before she leaves the clinic.

